Audits
NHIVNA conducts audits to assess and improve HIV nursing care standards, ensuring best practices are implemented across healthcare settings. Through systematic evaluations, NHIVNA identifies areas for enhancement and promotes high-quality, evidence-based care for people living with HIV.
A National Nurse-led Audit of the Standards for Psychological Support for Adults Living with HIV
NHIVNA is delighted to announce a national clinical audit of psychological support and emotional well-being among adults with HIV infection in the UK.
Click the button below to learn more about this audit.
An Audit of the HIV Nursing Competencies
NHIVNA conducted an audit of the HIV Nursing Competencies launched in 2007 to assess their impact and relevance in current practice.
Click the button below to read a report of the results of the Evaluation of the NHIVNA National HIV Nursing Competencies.
Audits… Why are clinical audits so important?
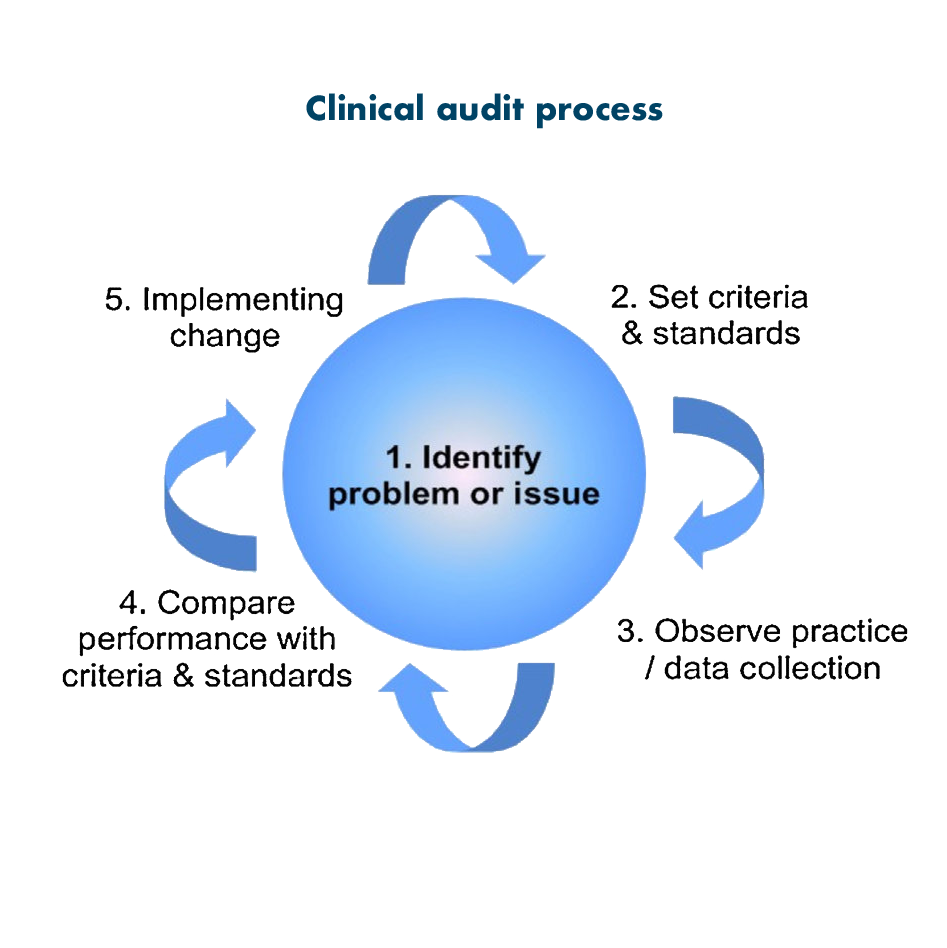
Clinical audit definition: Clinical audit is the process formally introduced in 1993 into the United Kingdom’s National Health Service (NHS), and is defined as “a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change”.
The key component of clinical audit is that performance is reviewed (or audited) to ensure that what should be done is being done, and if not it provides a framework to enable improvements to be made.
The clinical audit process seeks to identify areas for service improvement, develop and carry out action plans to rectify or improve service provision and then to re-audit to ensure that these changes have an effect.
Types of clinical audit
The place of clinical audit in modern healthcare
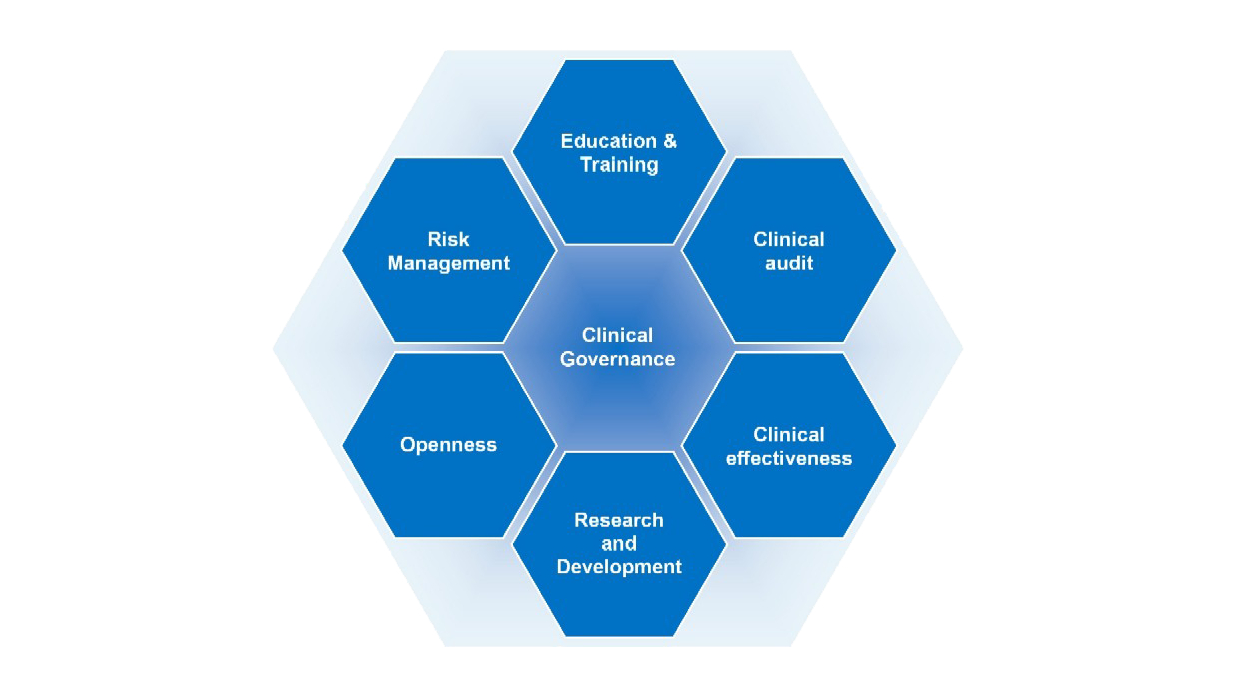
Clinical audit comes under the Clinical Governance umbrella and forms part of the system for improving the standard of clinical practice.
Clinical Governance is a system through which NHS organisations are accountable for continuously improving the quality of services, and ensures that there are clean lines of accountability within NHS Trusts and that there is a comprehensive programme of quality improvement systems.
The six pillars of clinical governance include:
- Clinical Effectiveness
- Research and Development
- Openness
- Risk Management
- Education and Training
- Clinical Audit
Clinical Governance
Clinical audit was incorporated within Clinical Governance in the 1997 White Paper, “The New NHS, Modern, Dependable”, which brought together disparate service improvement processes and formally established them into a coherent Clinical Governance framework.
Clinical audit is an essential and integral part of clinical governance.
Evidence based practice
What is evidence -based practice (EBP)?
Many terms are used in relation to evidence-based practice, evidence based nursing, evidence based nursing practice, evidence based medicine and evidence based healthcare.
Evidence based practice originated in medicine in 1992, since that time it has been gaining momentum in other disciplines, like nursing. More information about the development and history of evidence -based practice can be found at www.cebm.net/
Evidence-based practice (EBP) involves complex and conscientious decision-making, which is based not only on the available evidence but also on patient characteristics, situations, and preferences. It recognizes that care is individualized and ever changing and involves uncertainties and probabilities.
Most commonly used definition
Evidence-based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available clinical evidence from systematic research. (Sackett et al., 1996).
In the good old days when we asked why something was done in a particular way a nurse’s mantra was ‘sister says so’ or ‘we’ve always done it this way’. This is no longer sufficient and there is an expectation that strong evidence must underpin nursing practice.
Nurses need to make sure that the evidence they use is relevant to the practice of nursing. There is a range of evidence that can inform practice, personal experiences and reflections, literature, research, audit, policy, guidelines and clinical expertise all of which has its place within EBP.
Categories of evidence- a rating system for the hierarchy of evidence
The basic principles of evidence-based practice are that practical decisions should be made based on research studies and these studies are selected and interpreted based on the evidence based practice categories of evidence.
- Level one – Evidence from systematic reviews or Meta analysis of all relevant randomized control trials (RCT)
- Level two – Evidence obtained from well-designed RCT’s
- Level three – Evidence obtained from well-designed control without randomization
- Level four – Evidence from well-designed case control or cohort studies
- Level five – Evidence from systematic reviews of descriptive and qualitative studies
- Level six – Evidence from single descriptive or qualitative studies
- Level seven – Evidence from expert opinion, authorities and/or reports from expert committees.
Challenges with evidence based practice
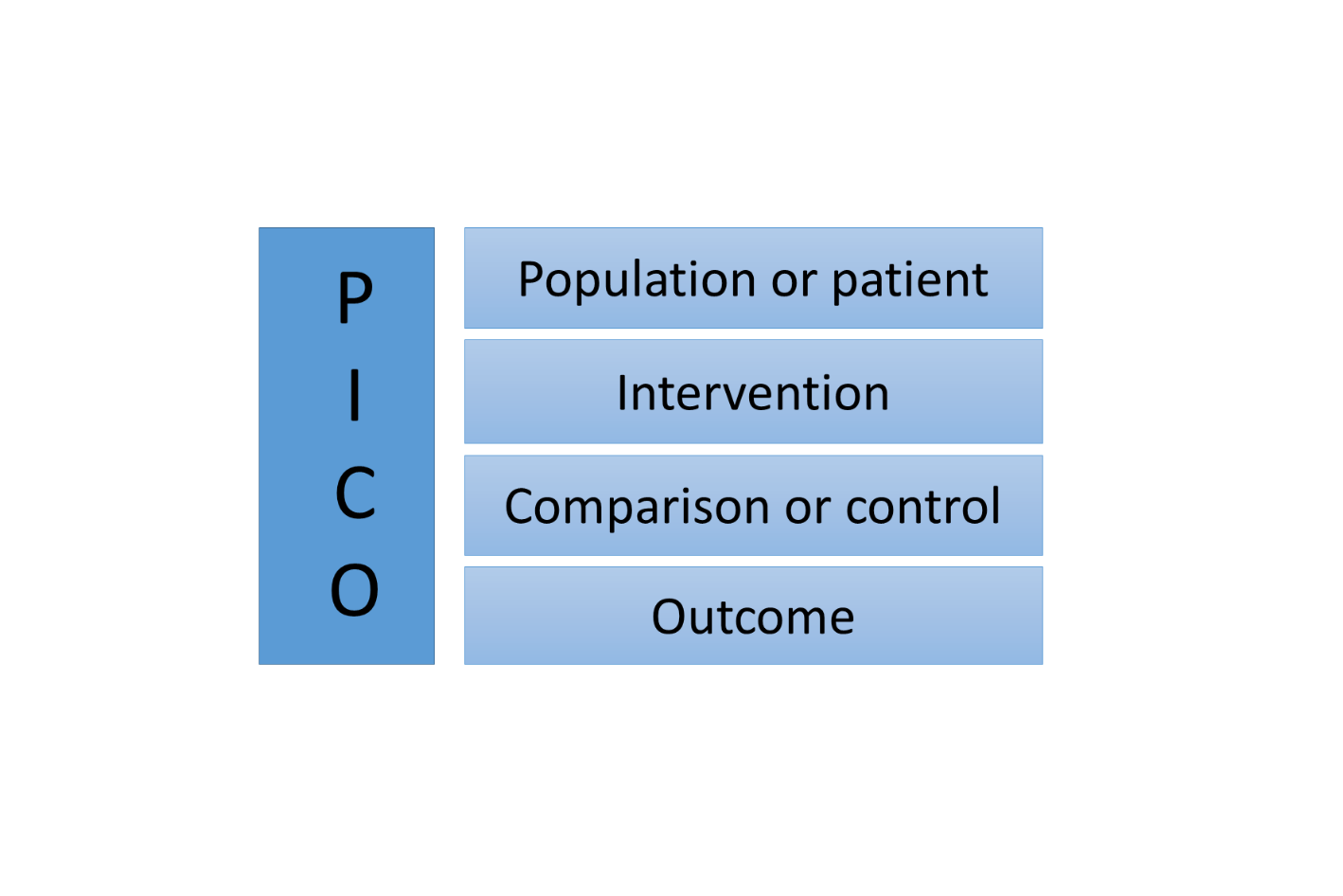
Evidence retrieval is one of the most common challenging issues with evidence based practice within a clinical settings learning to frame a question, so that an appropriate literature review can be performed .The following acronym is used to help practitioners remember the key components required and is called the ‘PICO” model.
P = Who is the Patient Population?
I = What is the potential Intervention or area of Interest?
C = Is there a Comparison intervention or Control group?
O = What is the desired Outcome?